Tomography has been frequently used and recognized as a key component for structural research in Life Sciences1,2. Here, the application of tomography was performed to assist in the accurate diagnosis of primary ciliary dyskinesia (PCD).
PCD belongs to a family of genetically heterogeneous disorders of motile cilia with a broad range of phenotypes, however, to a large degree also include mutations in the gene coding for the ciliary dynein arms3.
Typically, the workflow, when diagnosing a case suspected of PCD, necessitates scanning great numbers and/or large areas of plastic resin-embedded and traditionally stained thin sections while searching for axial cross-sections through cilia from which a diagnosis is made. The comparatively low appearance of almost perfect axial cross-sections of cilia has motivated the investigation and question, can tomography be applied to this field and help accelerate diagnosis? While tomography has been applied to PCD before4, it has not been established in applications as a standard diagnostic tool.
Specimens from cultured epithelium cells from both a healthy human subject and a patient suffering from PCD were immersed in 2% paraformaldehyde with 2% glutaraldehyde and 0.5% tannic in phosphate buffer; this is known to best stabilize and fix microtubular structures. Post-staining of silver sections with uranyl acetate and lead citrate was performed for microscopy. Tomography was carried out using a JEOL JEM-1400 transmission electron microscope operating at 120 kV using SerialEM to obtain the tilt series (+/- 60° at 1.5-2° intervals)5. Subsequent processing of the tilt series was performed using IMOD6.
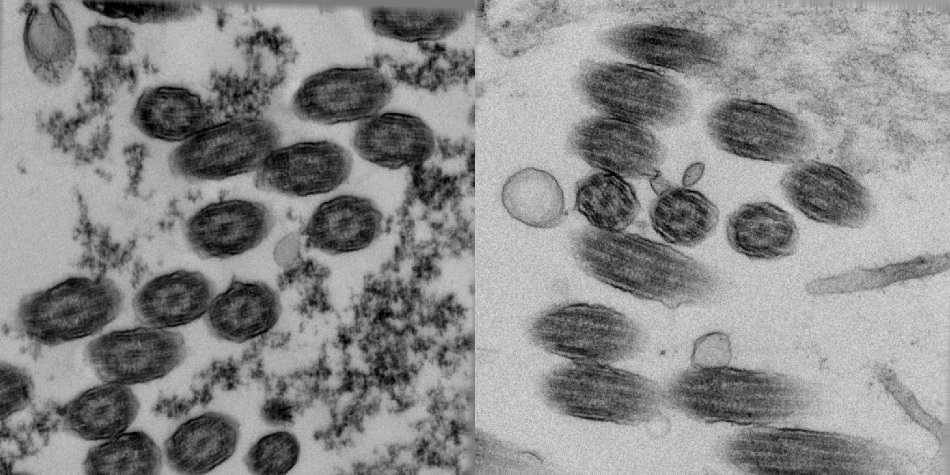
Figure 1. Untilted views of epithelial brush borders of healthy (left) and PCD-afflicted individuals (right).
Figure 1 exhibits a series of image fields of epithelial brush borders from healthy and PCD-cases featuring many cilia. Typically, the fields from the untilted views from the tilt series would not be enough for an accurate diagnosis, as the cilia would fail to reveal the proto-typical pattern.
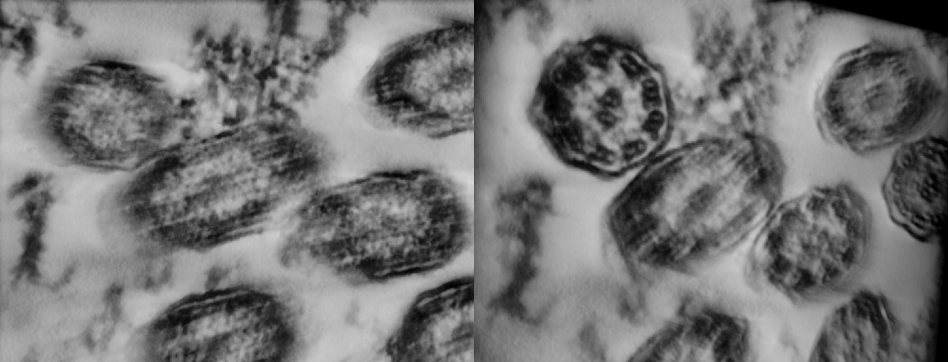
Figure 2. Close-ups of the reconstruction of cilia of a healthy individual untilted (left) and tilted to reveal the proto-typical view used for diagnostics (right). The tilt of the reconstruction was chosen to reveal the pattern in the upper left cilia.
Figure 2 demonstrates close-ups from the three-dimensional reconstruction produced using the tilt data of a healthy individual. This particular view clearly indicates glancing cross-sections through several cilia. Yet, the 3D reconstruction can be simply tilted in the computer to exhibit the proto-typical pattern with, among other features, connectivity of the dynein arms evidently shown.
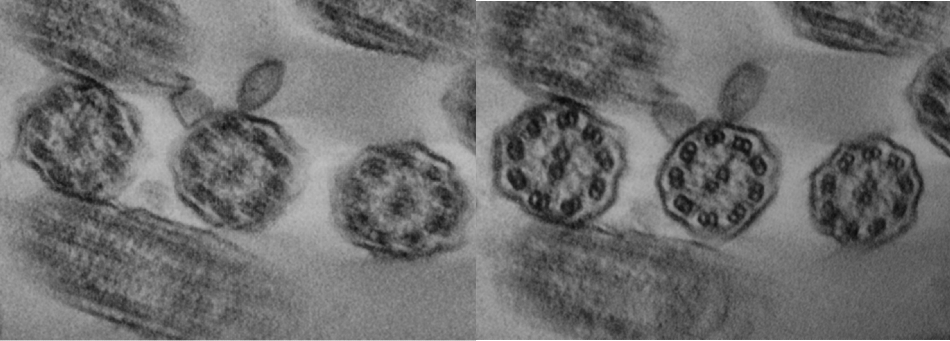
Figure 3. As in figure 2, but now from a PCD-case.
Likewise, Figure 3 illustrates the PCD-case, at which point resolution of the tilting of the reconstruction of the disconnected dynein arms is clear. It should be noted that the data was acquired in less than 30 minutes per case and the reconstructions were also achieved in under 30 minutes suggesting a diagnosis in under 1 hour. This vital data illustrates a proof of concept to the application of tomography to diagnosing PCD cases.
References and Further Reading
- Frank, J., Electron Tomography: Methods for Three-Dimensional Visualization of Structures in the Cell, 2nd ed., Springer, Albany, NY (2006).
- McIntosh, JR., Cellular Electron Tomography in: Methods in Cell Biology Series, Vol. 79, Elsevier, Amsterdam (2007).
- Leigh, MW et al., Genetics in Medicine 11 (2009) 473.
- O’Toole, E.T. et al., Microsc. Microanal. 14 (Suppl 2) (2008) 1476CD.
- Mastronarde, D.N., Microsc. Microanal. 9 (Suppl. 2) (2003) 1182CD.
- Kremer J.R. et al., J. Struct. Biol. 116 (1996) 71.
Acknowledgments
Produced from materials originally authored by J. Brink* and J.L. Carson** from:
*JEOL USA Inc., Peabody MA 01960
**University of North Carolina at Chapel Hill, Chapel Hill NC 27599.

This information has been sourced, reviewed and adapted from materials provided by JEOL USA, Inc.
For more information on this source, please visit JEOL USA, Inc.