| Prior to the early to mid 80s, condoms were low profile, undervalued articles. Their primary use revolved around the avoidance of pregnancy. Their function in helping to prevent sexually transmitted diseases (STDs), although recognized since Roman times, was not a major consideration among the general public. The advent of Acquired Immunodeficiency Syndrome (AIDS), coupled with increased incidence of STDs and the need to publicise effective means of avoiding infection, led to a much more open discussion of sexual matters. This brought the subject of condoms out of the barber’s shop and into the public arena. Condoms are no longer under-the-counter ‘johnnies’ or ‘rubbers’ but are classified medical devices and their production and sale are highly regulated activities. Standards Many countries have operated national standards on condoms for a long period of time, but in recent years standards have become much more demanding, reflecting the increasingly more important profile of the product. In 1990, ISO the International Standards Organisation, published a standard for condoms, which had previously been debated in draft for many years The European Commission has since followed suit and the CEN standard (EN 600) has now been approved and is expected to appear shortly. By mid 1998, all condoms sold in the European Union must comply with the requirements of the Commission’s Medical Device Directive and carry the CE marking. Origins of Condoms The origin of the use of condoms, or sheaths, for contraceptive or prophylactic purposes is literally lost in antiquity. Legend has it that King Minos of Crete used a goat’s bladder. Bladders were certainly used by the Romans for protection against infection. Elsewhere, other societies had recourse to alternative solutions: the Chinese used oiled silk and the Japanese used leather or, for their ‘Kabuta-gata’, a cap of tortoiseshell! The use of condoms is well documented from the Renaissance onwards. A linen sheath was designed in 1564 by the Italian physician, Gabriello Fallopio, but the name ‘condom’ was first used in print in 1717 by Daniel Turner, writing about venereal disease. This followed an allusion in The Tatler magazine that a Dr Condom had helped Charles II to avoid adding to his already large number of illegitimate heirs by recommending it. By the end of the eighteenth century, there was a thriving business in converting sheep’s caeca into so-called skin condoms. Both Boswell and Casanova are recorded as having made extensive use of such devices. The Advent Rubber Condoms Skin condoms continued to be used extensively and, indeed, it is still possible to buy condoms made from animal intestines. However, the cultivation and exploitation of the rubber tree, (Hevea brasiliensis), from the 1870s onwards eventually provided a much more suitable and controllable material. After early attempts at moulding from crepe rubber, a process of dipping a condom-shaped former in solutions of natural rubber in a petroleum solvent, followed by solvent evaporation and vulcanisation, was used successfully for many years, in spite of its tedious and hazardous nature. This process became obsolete after 1930, when natural rubber latex began to be shipped in concentrated form from South-East Asia to America and Europe. Now, by compounding the latex with vulcanising additives, antidegradants, and the like, it became possible to manufacture not only condoms, but also other thin-film rubber articles, such as gloves and balloons. Vulcanised films of natural rubber latex have outstanding elastic properties, such as tensile strengths of over 30MNm-2 at a breaking elongation in excess of 800%. Condoms could now be made thinner and stronger than before and could be coloured at will. Methods of surface texturing were also devised. The annual production of natural latex condoms reached a total of 8.5 billion units in 1993, but so lightweight are they (1.5g) that this represents less than 13,000 tonnes of rubber. Condom Production The same basic dipping process is in use today, although it has been extensively refined and automated. Shaped glass formers on an endless chain drive are dipped at controlled speed and temperature into a tank of compounded latex. When the formers leave the tank they are covered with a thin coating of latex, figure 1. | 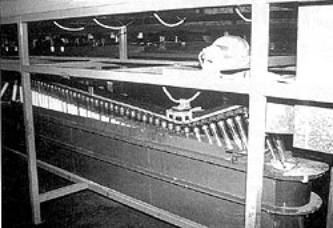
| | Figure 1. Condom formers entering and leaving the dipping tank. | The formers are rotated and partially or completely inverted to distribute the latex over the surface to give a coating of uniform thickness. The formers then pass through a heated chamber to dry the coating. Usually, the formers are then passed through a second latex tank, followed by drying, to give a thicker film. The upper end of the film is rolled down to form a strengthening rim, known as the bead, at the open end of the condom. The formers then pass through an oven, where drying and vulcanisation are completed. The condoms are stripped from the formers by brushes or jets of water, treated to prevent them sticking to themselves (usually by applying a pharmacologically safe powder and/or silicone oil) and tumble-dried. Testing Methods All the finished condoms are tested for ‘pin-holes’, usually by an electronic test that applies a fixed voltage across the film thickness. If any current is detected, the condom is rejected. Those passing the test are rolled and packaged individually in a foil pack. They may be packed dry or with an added lubricant, which may contain spermicide. Rigorous quality control is essential for the production of high quality condoms. In some countries, a batch of condoms can be released for sale only after a sample of the batch has been tested independently against the appropriate national standard. These tests are carried out both on freshly packaged condoms and on packed condoms that have been subjected to a short period of artificial ageing. Different national standards have different requirements but all include an assessment of dimensions, tensile properties, incidence of holes, and bursting properties. Currently, two methods of testing for holes are practised. Both depend upon filling the condom with water and detecting leakage either electrically or by observation. Both tests have drawbacks and a major EC-funded project is at present under way to assess the relative merits of each test. Some manufacturers and research organisations are continuing the search for a simple, reproducible, and reliable test. The air-inflation test has now been widely adopted by national standards bodies and is required by both ISO and CEN standards. Typically, a latex condom can be inflated to 40 litres before bursting, figure 2. However, there is still much controversy about how effective the air burst test is in predicting potential condom failure in use and there is much debate regarding the minimum requirements for the bursting pressure and volume that should be specified. The current minimum burst volume requirement of 16 or 18 litres would appear to be more than adequate for most men. | 
| | Figure 2. Condom burst testing using the sir inflation test. | Barrier Properties It has also been necessary to assess how effective the condom is at preventing the passage of human sperm and the organisms responsible for the various STDs. Due to the fact that sperm are much larger than many micro-organisms that transmit diseases, it is clear that retaining sperm is the least demanding requirement. Furthermore, evidence indicates that an intact natural rubber condom free from defects provides a complete barrier to sperm. Failure Rates Clinical studies conducted in the UK between 1960 and 1980 showed very low failure rates, from 0.4-1.4 pregnancies per 100 women-years of use. Some of these failures will have been due to breakage of the condom during intercourse. One US consumer survey of nearly 3300 people reported condom breakage incidence as less than 1% and a more recent user study conducted in the UK yielded an average breakage rate of only 0.3% among couples using condoms as the sole contraceptive, indicating modern condoms are effective and reliable. Reasons for Failures There are strong indications from other studies that even these low figures are not entirely due to the properties of the condom itself. Breakage and slippage of condoms seem not to be randomly experienced by all users. A relatively small percentage of couples report higher than average breakage and slippage rates. Many failures can be attributed to condom misuse, including the application of an oil-based lubricant (which very quickly destroys condom strength), damage from fingernails or rings, incorrect donning or poor withdrawal technique, and even re-use of a condom. Thus consumer education on the proper use of condoms is essential. Sexually Transmitted Diseases While there are several effective means of preventing or reducing the incidence of pregnancy arising from intercourse, there are far fewer reliable options for avoiding transmission of STDs. Epidemiological studies have shown that condoms protect against a wide range of STDs, including syphilis, gonorrhoea, chlamydia, herpes, and hepatitis B. Actual in use studies of the condom as a barrier to organisms responsible for STDs have been limited to the Human Immunodeficiency Virus (HIV). A clinical study of 256 heterosexual couples, where only one partner was HIV-positive, was carried out in France. None of the 124 HIV-negative male or female partners who consistently used condoms became infected over the 22 months of the study in a total of about 15,000 episodes of intercourse. In contrast, 12 of the remaining 121 partners who either did not use condoms or used them inconsistently became infected. Allergic Reactions Natural rubber condoms may give rise to skin irritation or allergic reactions in sensitive individuals. These conditions originate either from chemicals added to vulcanise the rubber or from the proteins present in natural rubber latex, which is derived, after all, from a plant material. In actual fact, allergy has not proved a significant problem in condom use, except for a very small group of particularly sensitive individuals. The incidence of such medical conditions has been most prevalent in users of rubber latex gloves, possibly because gloves are typically worn for longer periods and, being thicker, require more effective washing to remove residual chemicals and proteins. Physiological Responses The physiological responses to natural rubber articles are of three types: irritation, delayed contact dermatitis (type IV allergy), and immediate (type I) allergy, table 1. | | | Irritation (contact dermatitis) | Point if contact | Itching, reddening, swelling, blistering | Physical or chemical damage to skin | Minutes to hours | Adequate skin care. Avoid source of irritation | | Delayed contact dermatitis (type IV allergy) | Point of contact and local area | Itching, reddening, blistering, peeling | Chemical allergens, often accelerators of vulcanisation | Up to 48 hours | Avoid all offending accelerators/ allergens | | Immediate allergy (type I) | Any body part | Itching, weal & flare, hives, runny nose and eyes, wheezing, asthma, anaphylaxis | Water-soluble proteins in natural rubber latex | Minutes up to 1 hour | Avoid any contact with natural rubber materials and products | Irritation is rarely encountered with condoms and, when it is, is more likely to be due to added substances such as fragrances or lubricants than to components of the rubber. What are Allergic Reactions? Allergic responses are usually an overreaction of the immune system to otherwise harmless substances. Individuals who may have a predisposition to allergy will, on initial contact with a particular material, show no sign of adverse reaction. However, this contact may sensitise the individual so that subsequent contact with the material leads to severe effects, both at the point of contact (usually skin responses) or remotely (e.g. rhinitis, conjunctivitis, wheezing and asthma). In extreme cases of type I allergy, the reaction may be life-threatening anaphylaxis (constriction of smooth muscle, reduction in blood pressure, breathing difficulties). This allergy is closely analogous to the well-known nut and fruit allergies. Allergies to Vulcanising Chemicals The type IV allergy to some vulcanising chemicals has been known for a long time but latex protein (type I) allergy was not recognised until 1979 and then only developed into a problem of any significance in the late 1980s. The reasons for its appearance cannot be stated with certainty but it seems likely that the advent of HIV and the explosion in examination glove usage led to a burgeoning of new and inexperienced glove manufacturing companies, which resulted in poorly washed products appearing on the market. The consequence has been that increasing numbers of healthcare workers, particularly in the USA, have been sensitised to natural rubber protein through use of latex examination gloves. It appears that, in most cases, initial sensitisation to both type IV and type I allergens arises from occupational use of medical gloves, rather than to condom use per se. However, subsequent use of a condom containing the same allergen may then result in an allergic reaction. For cases of type IV allergy, an effective solution is often to use only those products marketed as being low in residual concentrations of accelerators. Such so-called ‘hypoallergenic’ or ‘low allergy’ condoms can often be tolerated by all but the most highly sensitive. However, any individual sensitised to latex protein is best advised to avoid further contact of any sort with natural rubber. For such people, use of latex condoms will carry a potential risk. New Condom Materials Market research has shown that a major excuse for not using condoms is that they reduce sensitivity and feeling during intercourse. The wall thickness of latex condoms is typically 0.06mm 0.07mm. In order to reduce this significantly without sacrificing safety, stronger materials are required. This has led many manufacturers over the years to start investigating alternative materials. More recently, the emergence of the latex protein allergy problem has given added impetus to this search. Polyurethanes In the 1980s, London International Group (LIG) started a programme directed at identifying suitable synthetic rubbers for condoms. It quickly became apparent that none of the commercially available elastomers was suitable, either because they were not readily processable or because their physical properties were not appropriate. They were either strong but too hard and stiff, or soft but weak. However, polyurethanes were identified as the materials of choice and a specification was developed for an optimal polyurethane elastomer. This unique material was then developed in partnership with a major polyurethane manufacturer. The polyurethane used has been given the brand name Duron. With a tensile strength twice that of natural rubber latex film, it has allowed LIG to make condoms that are significantly thinner than conventional high quality latex condoms but just as durable. Duron is also odourless, tasteless, and colourless and in biocompatibility testing has been shown to be non-allergenic. The world’s first commercial male polyurethane condom, Avanti, made from Duron, was launched in the west-coast states of the USA in November 1994. Other manufacturers have since received clearance from the FDA to market condoms from other materials. Clinical Results Avanti condoms have been subjected to extensive testing, both in laboratory and in clinical studies in a number of countries. The in-use clinical studies have shown Avanti condoms to be equivalent to high quality latex condoms in terms of breakage and slippage rates, and laboratory studies have shown the condom material to be a barrier to organisms much smaller than HIV (120nm) or even Hepatitis B virus (40nm). Large-scale clinical studies are also under way, directed at determining the contraceptive efficacy of the Avanti condom. Advantages of Polyrethane Condoms The in-use studies have also demonstrated that the thinner Avanti condom is significantly more sensitive and comfortable than the conventional latex condom. It was also found to be agreeable in feel and appearance, and generally much more acceptable to users. A condom with these attributes should encourage more people to use condoms for protection, both against pregnancy and against the transmission of STDs. The Avanti condom is also suitable for use by people who are latex-sensitive since it is free from latex proteins and from the ingredients used in the compounding and curing of latex. Materials for the Future The Avanti condom is undoubtedly an indicator for the future. A number of condoms made from other synthetic materials are under development by other companies and research organisations. Whilst some of these are based upon polyurethanes, others are based on polymers such as the block copolymers, SBS, SEBS and SIS. There will surely be others. Andare avanti! |