The drawbacks of traditional arrhythmia diagnosis are the time-consuming intermittent clinical examinations, lack of quantitative data, mismatch between cardiac monitoring sensors and human skin, and the requirement of expert evaluation.
However, modern flexible, wearable, bioelectric, ultrasonic, optoelectronic, and mechanoelectrical sensors and machine learning algorithms have alleviated this problem. In a recent study published in the journal Materials, researchers from the USA analyzed the current advancements in flexible wearable sensors for cardiac heart-rate variability monitoring and arrhythmia detection.
What is Arrhythmia?
Arrhythmia is a cardiovascular disease in which the electrical pulses of the heart do not function properly, causing the heart to beat either too slow, too fast, or skip beats. In 2018, more than 500,000 American deaths were due to inherent arrhythmia as a contributing factor. Arrhythmia can be classified into two types based on the nature of the effect on heart impulses – impulse-production arrhythmia and impulse-conduction arrhythmia.
Impulse-production arrhythmias can be classified into non-sinus rhythm, fibrillation, tachycardias, bradycardias, and flutter. Atrial fibrillation is the most common arrhythmia, which occurs when the electrical pulses between the atria do not synchronize with the pulses in the ventricles.
Ventricular fibrillation occurs when there is a mismatch of pulses between the right and left atria, which renders the heart unable to pump blood to the body. Tachycardias occur when the heart is beating too fast (>100 beats per minute), whereas bradycardias occur when the heart is beating too slow (<40 beats per minute).
Impulse-conduction arrhythmia types include atrioventricular block due to impulse blockage between the atria and ventricles, bundle branch block due to blockages in the pathways in the heart, Wolff-Parkinson-White syndrome due to the formation of additional electrical pathways, and escape beats.
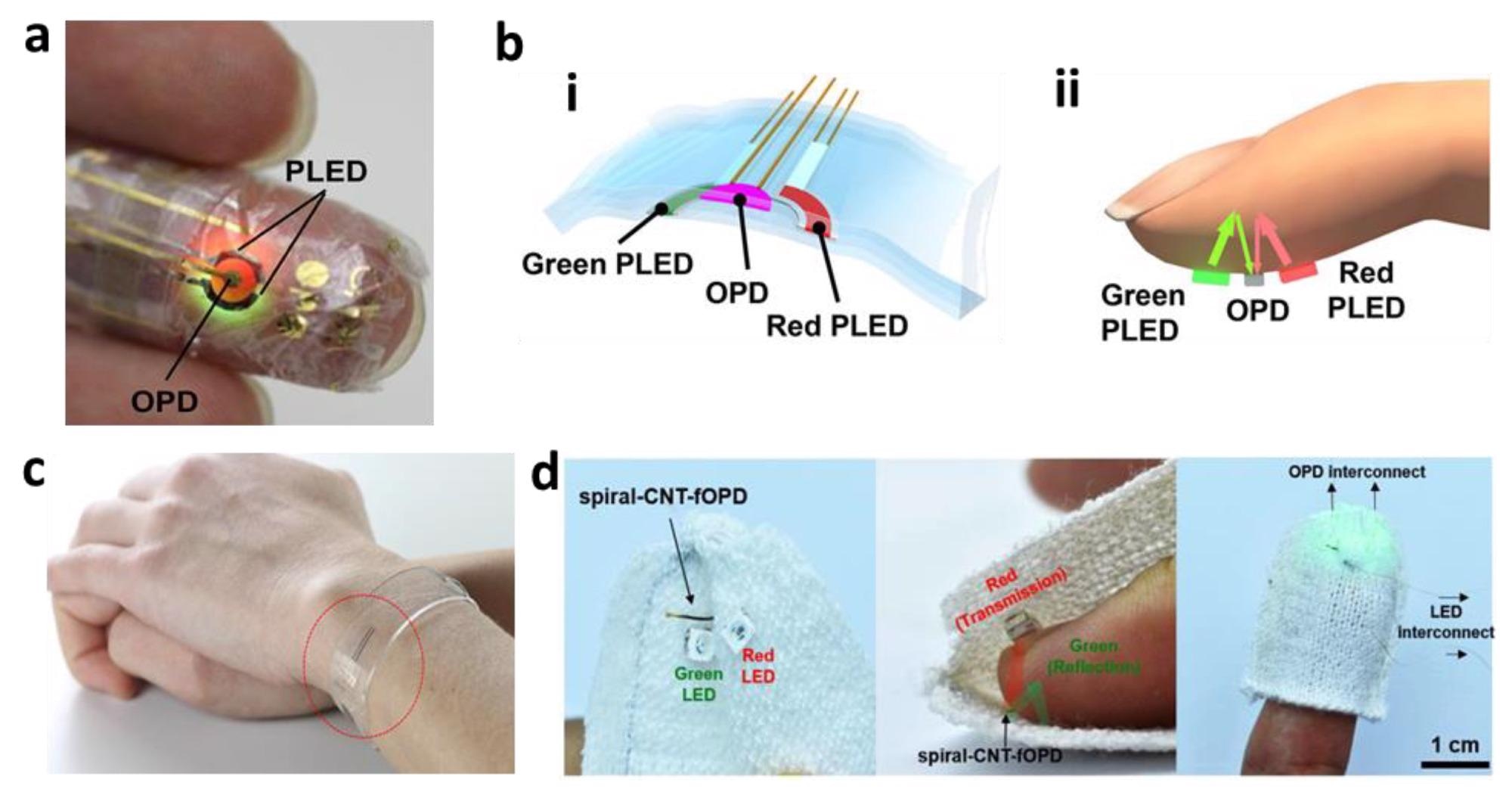
Photoplethysmography. (a) Photo of an ultra-flexible organic optical sensor. (b) Illustration of polymer LED (i) and organic photodiode (ii) pulse oximeters. (c) Photo of a graphene-based flexible sensor in a heart-rate monitoring bracelet. (d) Photos of CNT-based microelectrodes for a fiber optoelectronic device. Image Credit: Guess, M. et al., Materials
Diagnosis of Arrhythmia
Traditionally, arrhythmias have been diagnosed by expert medical professionals based on a patient’s medical history, clinical examinations, and qualitative data based on very few quantitative data. The most commonly used instrument for this purpose is electrocardiography (ECG). However, its bulkiness, intermittent (not continuous) clinical recording, reliance on wired leads, and signal deterioration due to the drying and shaking of the conductive gels have caused disrupted data collection.
The new generation of flexible devices is a promising alternative to these rigid devices due to several additional benefits such as their low cost, faster manufacturing, portability, the elimination of relative motion by increasing sensor-to-skin adhesion, and provides additional information such as ultrasound, photoplethysmography, seismocardiography, and ballistocardiography to study electromechanics of the heart.
Cardio Signals and Corresponding Instruments
The bioelectric signals are detected by ECG using 12 leads, 10 electrodes, and five types of waves viz. P, Q, R, S, and T. The P wave represents atrial depolarization, the QRS complex wave represents ventricular depolarization and ventricular contraction, and the T wave represents ventricular diastole and ventricular repolarization.
Moreover, single-lead cardiovascular patches have become more clinically suitable for detecting arrhythmias compared to a 12-lead Holter ECG monitor. The conductive Ag/AgCl metal electrodes with high Young’s modulus can be replaced with conductive polymers having low Young’s modulus such as polyethylene terephthalate (PET), polystyrene trans acid (PEDOT:PSS), poly (3,4-ethylene dioxythiophene), and polydimethylsiloxane (PDMS).
Additionally, the incorporation of activated carbon and metal nanoparticles networks can increase the conductivity of these polymers. This strategy eliminates the use of metal electrodes and conductive gels.
Photoplethysmography (PPG) is an emerging optoelectronic signal-based alternative to ECG for cardiovascular monitoring due to its compact size and ability to capture many different physiological parameters using red and near-infrared (NIR) LEDs.
It consists of one set of LEDs and another set of photodiodes that detects changes in light intensity depending on the volumetric changes in the veins and arteries during pulses. It is also used to measure blood oxygen saturation (SpO2), blood pressure, heart rate, and respiratory rate. Polymer LEDs (PLEDs) consisting of light-emitting polymers and indium tin oxide (ITO) electrodes, and organic photodiode (OPD) fabricated with a poly(3-hexylthiophene) (P3HT):(6,6)-phenyl-C61-butyric acid methyl ester (PCBM) active layer, are effectively suppressing fundamental motion-artifact noises.
Moreover, ultrasonic signals using lead zirconate titanate (PZT) piezoelectric transducers, seismocardiography (SCG) based on polyvinylidene fluoride (PVDF), and Ag/AgCl ink-based electrodes are suitable alternatives. Additionally, machine learning models such as support vector machine (SVM), decision tree (DT) models, multilayer perceptron (MLP), convolutional neural network (CNN), recurrent neural network (RNN), deep belief network (DBN), gated recurrent unit (GRU), and long short-term memory (LSTM), have been applied to detect arrhythmia effectively.
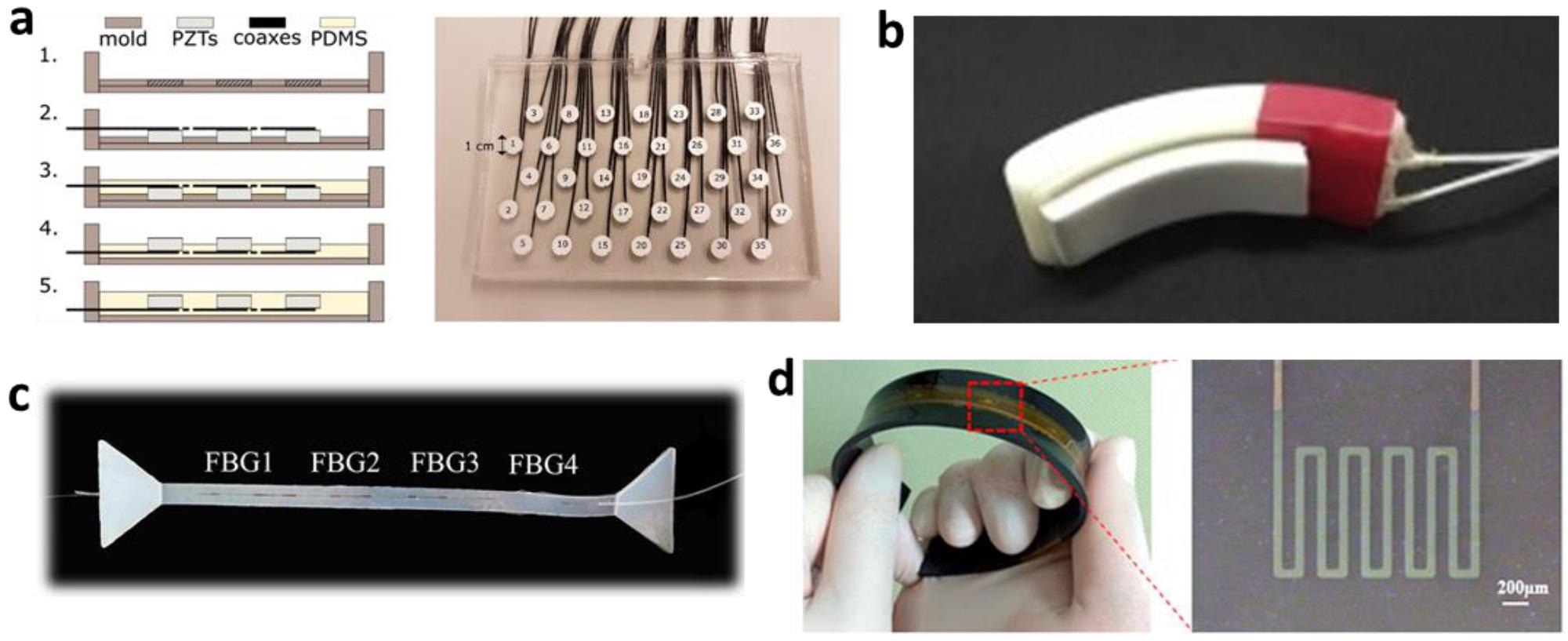
(a) Fabrication processes (left) and photo of a fabricated ultrasonic transducer (right). (b) Photo of a finger-worn SCG sensor. (c) Photo of a skin-like SCG sensor with fibers. (d) Flexible strain sensor for heartbeat monitoring. Image Credit: Guess, M. et al., Materials
Conclusions
To conclude, researchers analyzed different types of cardio signal detection strategies and instruments with current trending alternatives for arrhythmia diagnosis. The bioelectric, optoelectric, mechanoelectrical, and ultrasonic signal detection using conducting polymer and piezoelectric composites, miniaturization, impedance control, and increased sensor-to-skin contact quality can help in early arrhythmia detection.
Reference
Guess, M., Zavanelli, N., Yeo, W., Recent Advances in Materials and Flexible Sensors for Arrhythmia Detection. Materials, 2022, 15, 724. https://www.mdpi.com/1996-1944/15/3/724
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.