Foot pathology requires unique customization in clinical practice, which must be patient- and disease-specific. Traditional methods for making custom functional foot orthoses (FO) are still based on plaster casting and hand production; therefore, orthotic therapy is entirely dependent on individual practitioners' talents and competence. This makes the methods difficult to standardize and repeat, as well as costly, material-intensive, and time-consuming.
3D printing opens up new possibilities in producing patient-specific orthoses because it allows designers to address all of the limitations of current technologies. However, it has only been lightly explored in the podiatric field, and many aspects remain unmet, particularly in terms of customization, which necessitates the development of a protocol that covers all stages from patient scanning to manufacturing.

Figure 1. Comparison of ten plaster casts obtained after footprint recording with pinstripe and subtalar joint bandage in the neutral position (a neutral suspension cast).
About the Study
In this study, the authors presented a feasibility study that included interdisciplinary collaboration between industrial engineers and podiatrists. 3D foot scans were compared to traditional casting for patient-specific data collecting. A modeling generative design (GD) workflow was designed to develop a method that allowed for the easy creation of unique shapes, allowing the end-user or the podiatrist to customize the orthoses interactively.
A comparison of different printing materials was made to replicate the mechanical behavior of typical orthoses. The mechanical properties of cut and hand-shaped standard materials i.e., polycarbonate sheets, were compared to four groups of the 3D printed samples i.e., poly(acrylonitrile-butadiene-styrene) (ABS), poly(ethylene glycol) (PETG), poly(lactic acid) (PLA), and polycarbonate (PC) obtained by fused filament fabrication (FFF).
The team compared the 3D scanning of the foot to traditional casting for patient-specific data gathering. To allow podiatrists to readily build and interactively customize foot orthoses and a sensorized house slipper, a GD approach was devised.
The most commonly used 3D printing materials for making custom foot orthoses were compared. Scanning 10 plaster casts generated by the footprint recording with a pinstripe and subtalar joint bandage in a neutral position was used to make an initial comparison. Polycarbonate specimens were utilized as the gold standard in terms of mechanical behavior, and its mechanical behavior was favored for creating corrective insoles.
The researchers characterized the first failure stress as a change in slope in the stress/strain plot that was higher than 1% of the prior sample. The Young modulus was calculated using linear regression of the stress-strain curve in the 20% to 80% of the first failure stress range. The integral under the stress-strain curve until the first Failure stress arises helped calculate the first failure work. The integral under the stress-strain curve until the final failure was used to calculate the total work.
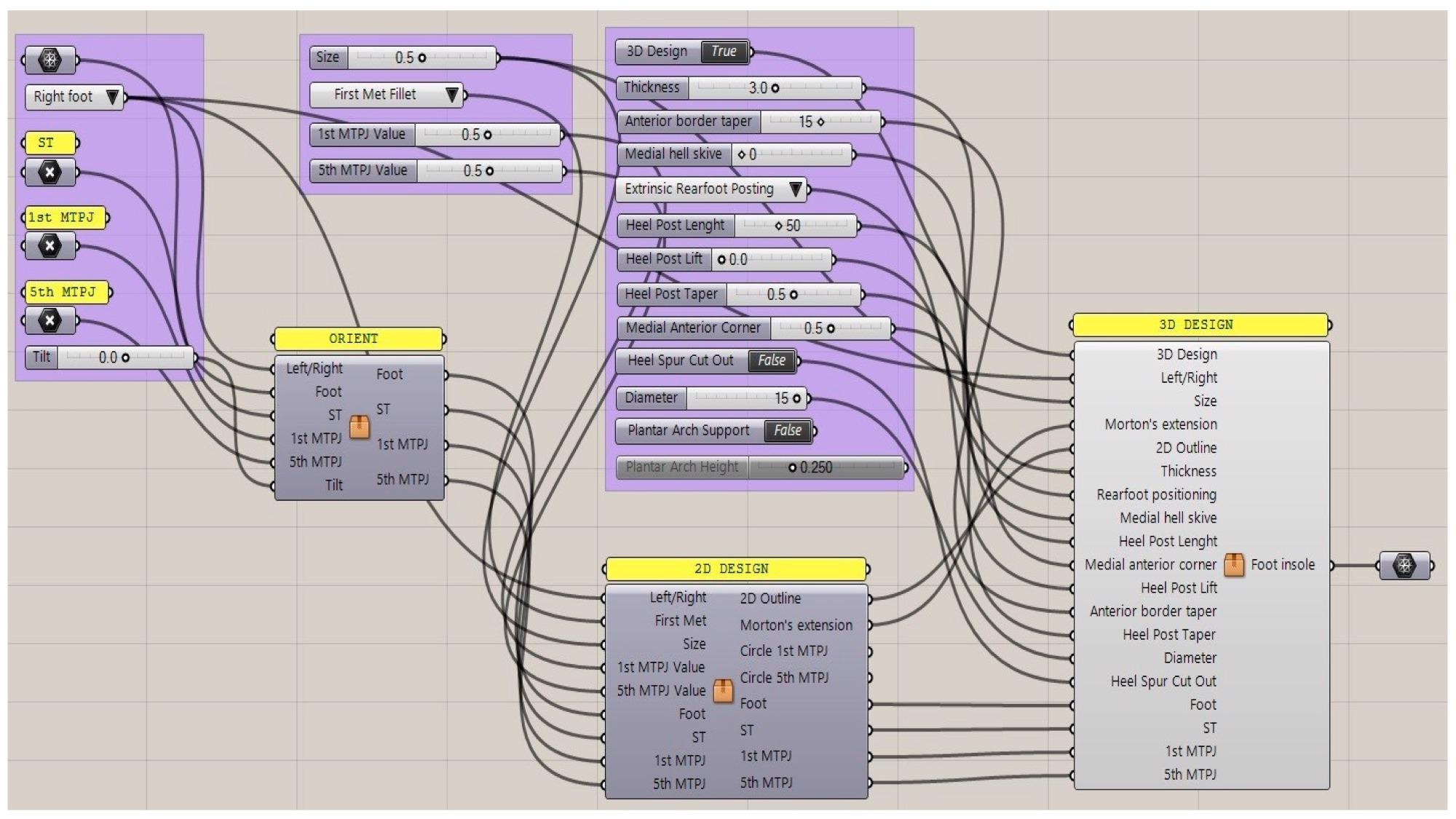
Figure 2. Generative design workflow with input data and sliders of the control panel for interactively modifying the foot orthosis and adding corrections (Grasshopper).
Observations
A customized foot orthosis could be designed by a non-experienced user in less than 5 minutes, according to the feasibility studies, which included medical staff. Differences between the foot plaster model prepared with the plaster slipper cast in the neutral position and the real foot model produced with 3D scanning could be attributed to the patient's non-stationarity during the acquisition process, which was limited by a locking system that prevented significant differences in the entire sole of the foot scan.
Podiatrists with modest computer-aided design (CAD) abilities could simply create and interactively customize foot orthoses to meet the clinical demands of their patients by using the established GD methodology. The complicated shape of the orthoses could be readily and swiftly recreated via 3D printing.
All of the printed materials reached lower yield stress and were less deformable when compared to polycarbonate sheets of the gold standard. There were no changes in any material as a result of the printing procedure. The different orientations of loads in identical 3D printed models generated in the same way in the 3D printer's building chamber could react differently. More testing was needed in terms of printing direction and mechanical loading conditions to determine which materials were most suited to everyday life and medical demands.
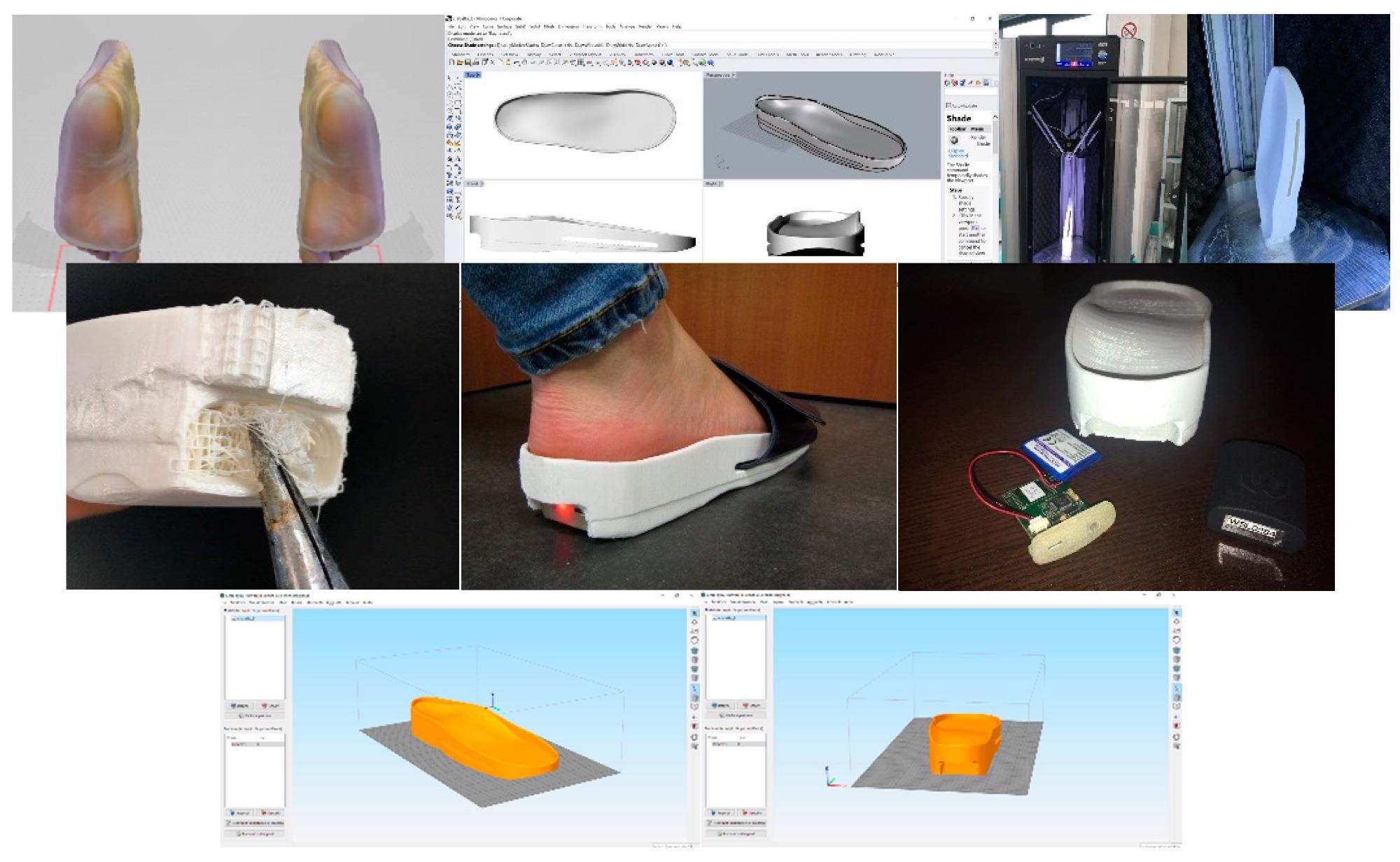
Figure 3. Key steps in the modelling process for the sensorized house slipper.
Conclusions
In conclusion, this study described a new technique for producing bespoke foot orthoses. The procedure was both cost-effective and simple to use for professionals. In terms of 3D scanning, it was demonstrated that the acquisition technique process was more accurate since the patient must be relaxed and their foot must be firmly secured in the neutral position, as opposed to 3D scanning of the foot without any foot locking device and with a handheld 3D scanner.
In terms of printing, it was proven that the choice of polymeric materials had a significant impact on the manufacturing process in terms of mechanical qualities.
The authors believe that the 3D digital approach opens up many new possibilities. To analyze the orthoses' behavior following simulated aging, a complete mechanical characterization was reported necessary.
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.
Source:
Brognara, L., Fantini, M., Morellato, K., et al. Foot Orthosis and Sensorized House Slipper by 3D Printing. Materials 15(12) 4064 (2022). https://www.mdpi.com/1996-1944/15/12/4064/htm.